ECG (EKG) Interpretation
As with all investigations the most important things are your findings on history, examination and basic observations. Having a good system will avoid making errors.
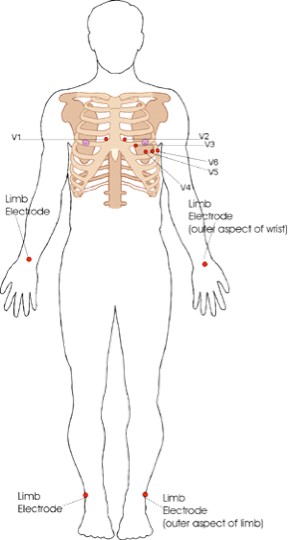
To start with we will cover the basics of the ECG, how it is recorded and the basic physiology. The 12-lead ECG misleadingly only has 10 electrodes (sometimes also called leads but to avoid confusion we will refer to them as electrodes).
The leads can be thought of as taking a picture of the heart’s electrical activity from 12 different positions using information picked up by the 10 electrodes. These comprise 4 limb electrodes and 6 chest electrodes.
Figure 1. Electrode positions on an ECG (EKG).
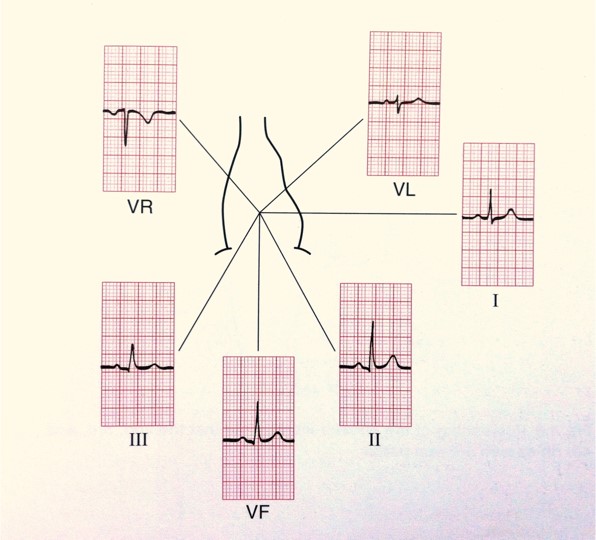
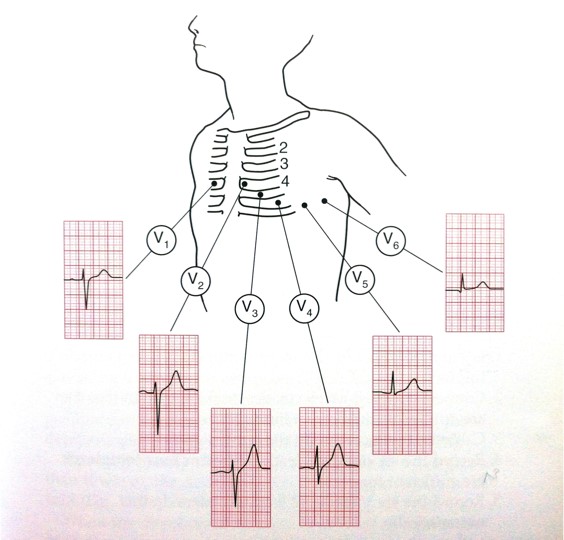
When electrical activity (or depolarisation) travels towards a lead, the deflection is net positive. When the activity travels away from the lead the deflection is net negative. If it is at 90 degrees then the complex is ‘isoelectric’ i.e. the R and S wave are the same size. This can often be seen in V4 (see Figure 3).
Figure 2. The electrical activity on an ECG (EKG).
Figure 3. The electrical activity on an ECG (EKG).
The areas represented on the ECG are summarized below:
- V1, V2 = RV
- V3, V4 = septum
- V5, V6 = L side of the heart
- Lead I = L side of the heart
- Lead II = inferior territory
- Lead III = inferior territory
- aVF = inferior territory (remember ‘F’ for ‘feet’)
- aVL = L side of the heart
- aVR = R side of the heart
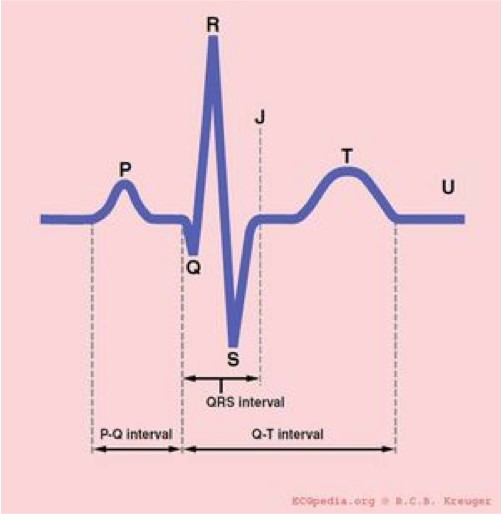
The ECG can be broken down into the individual components. For the purpose of this we will look at lead II (see Figure 4). All boxes are based on the assumption that the paper speed is running at 25mm/sec, therefore 1 large square is equivalent to 0.2 secs and a small square to 0.04 secs.
Figure 4. The segments of the ECG.
What do the segments of the ECG represent?
- P-wave: Atrial contraction
- PR interval: Represents the time taken for excitation to spread from the sino-atrial (SA) node across the atrium and down to the ventricular muscle via the bundle of His.
- QRS: Ventricular contraction
- ST segment: Ventricular relaxation
- T-wave: Ventricular repolarisation
Normal duration of ECG segments:
- PR interval: 0.12 – 0.2 secs (3-5 small squares)
- QRS: <0.12 secs (3 small squares)
- QTc: 0.38 – 0.42 secs
How to read an ECG
There are many different systems to interpret the ECG. This system ensures you will never miss anything:
- Patient details
- Situation details
- Rate
- Rhthm
- Axis
- P-wave and P-R interval
- Q-wave and QRS complex
- ST segment
- QT interval
- T-wave
These components will now be explained in more detail.
1. Patient details
- Patient’s name, date of birth and hospital number
- Location
- This becomes important as in the ED or acute medical setting doctors are often shown multiple ECGs. You need to know where your patient is in order to ensure that they can be moved to a higher dependency area if appropriate.
2. Situation details
- When was the ECG done?
- The time
- The number of the ECG if it is one of a series
- If you are concerned that there are dynamic changes in an ECG it is helpful to ask for serial ECGs (usually three ECGs recorded 10 minutes apart) so they can be compared. These should always be labelled 1, 2 and 3.
- Did the patient have chest pain at the time?
- Or other relevant clinical details. For example, if you are wanted an ECG to look for changes of hyperkalaemia, note the patient’s potassium level on the ECG.
3. Measuring the rate on an ECG
- Rate can be calculated in a number of ways:
- Count the number of QRSs on one line of the ECG (usually lead II – running along the bottom) and multiply by six.
- Count the number of large squares between R waves and divide 300 by this number (if the patient is in atrial fibrillation it is more accurate to report a rate range rather than a single value).
4. Assessing the rhythm on an ECG
- Is the rhythm regular or irregular? If it is irregular is it regularly or irregularly irregular?
- Rhythm can be difficult to assess especially in bradycardia or tachycardia. It may be helpful to use the ‘paper test’.
- To do this place a piece of scrap paper over the ECG and mark a dot next to the top of a QRS complex, draw another dot next to the top of the next QRS then slide the paper along the ECG. If the rhythm is regular you should see that your two dots match to the tops of the QRS complexes throughout the ECG.
5. Assessing the axis on an ECG
- Axis is the sum of all the electrical activity in the heart.
- The contraction travels from the atria to the right and left ventricles. As the left ventricle is larger and more muscular normal axis lies to the left (at -30 degrees to 90 degrees – see Figure 5).
- As a general rule if the net deflections in leads I and aVF are positive then the axis is normal.
- If lead I has a net negative deflection whilst aVF is positive then there is right axis deviation.
- If lead I has a positive deflection and aVF has a negative deflection then there is left axis deviation
- If you want to work it out more precisely you can use the method below:
- Count the number of small squares of positive or negative deflection in aVF and make a dot on the aVF axis (see Figure 5) moving a mm for each small square counted (e.g. x mm up for negative and x mm down for positive deflections).
- Count the number of small squares of positive or negative deflection in lead 1 and make a dot on the lead 1 axis moving a mm from the centre of the chart for each small square counted (e.g. x mm right for negative and x mm left for positive deflections).
- Draw a horizontal line through your lead 1 dot and a vertical line through your aVF dot then draw a line from this intersection back through 0 and this will give you the accurate axis.
Figure 5. The axis of the heart – a useful diagram for assessing the cardiac axis using the method above.
Causes of axis deviation
| Left axis deviation | Right axis deviation |
|
|
6. P-wave and PR interval
- Can you see a p-wave? If the rhythm is atrial fibrillation, atrial flutter or a junctional tachycardia you may not be able to.
- At this point you can also assess whether each p wave is associated with a QRS complex. P-waves not in association with QRS complexes indicate complete heart block.
- Assess p-wave morphology
- In some cases there can be a notched (or bifid) p-wave known as “p mitrale”, indicative of left atrial hypertrophy which may be caused by mitral stenosis. There may be tall peaked p-waves. This is called “p-pulmonale” and is indicative of right atrial hypertrophy often secondary to tricuspid stenosis or pulmonary hypertension.
- A similar picture can be seen in hypokalaemia (known as “pseudo p-pulmonale”).
- The PR interval may be prolonged in first degree heart block (described in more detail later).
- The PR interval may be shortened when there is rapid conduction via an accessory pathway, for example in Wolff Parkinson White syndrome.
- PR depression may be seen in pericarditis.
7. Assessing Q-wave and QRS complex
- Q-wave
- A q-wave is an initial downward deflection in the QRS complex. These are normal in left-sided chest leads (V5, 6, lead I, aVL) as they represent septal depolarization from left to right. This is as long as they are <0.04secs long (1 small square) and <2mm deep.
- If q-waves are larger than this or present in other leads they are pathological.
- QRS complex
- Width
- The QRS complex normally lasts for < 0.12 secs (3 small squares).
- Causes of a wide QRS:
- Bundle branch blocks (LBBB or RBBB)
- Hyperkalaemia
- Paced rhythm
- Ventricular pre-excitation (e.g. Wolf Parkinson White)
- Ventricular rhythm
- Tricyclic antidepressant (TCA) poisoning
- Shape and height
- The QRS may be small (or low voltage) in pericardial effusion, high BMI, emphysema, cardiomyopathy and cardiac amyloid.
- The QRS is tall in left ventricular hypertrophy (LVH)
- The criteria suggestive of LVH on the ECG is if the height of the R wave in V6 + the depth of the S wave in V1. If this value is >35mm this is suggestive of LVH.
- The QRS can also be tall in young, fit people (especially if thin).
- Width
8. ST segment
- The ST segment can be normal, elevated or depressed. To be significant the S-T segment must be depressed or elevated by 1 or more millimeters in 2 consecutive limb leads or 2 or more millimeters in 2 consecutive chest leads. Look out for reciprocal changes.
- ST elevation indicates infarction.
- ST depression is normally due to ischaemia.
- ST segment depression may also be seen in digoxin toxicity. Here the ST depression will be downsloping (sometimes known as the “reverse tick” sign).
NB: High-takeoff
- A mimic of ST elevation is high-takeoff. High-takeoff is also known as benign early repolarization.
- High-takeoff is where there is widespread concave ST elevation, often with a slurring of the j-point (start of the ST segment). It is most prominent in leads V2-5, is usually in young health people and is benign.
- The best ways to differentiate it from myocardial infarction are:
- The ST segments are concave; they are most prominent in V2-5; they have a slurred start (j-point); the ST elevation is usually minimal compared to the amplitude of the t-wave; there are no reciprocal changes; the ST segments do not change over time.
9. QT interval
- The QT interval is the time between the start of the q-wave and the end of the t-wave.
- The QT interval is corrected for heart rate giving the QTc.
- As a quick check, if the t-waves occur over half way between the QRS complexes the QTc may be lengthened
- Not an accurate method but very quick!
- As a quick check, if the t-waves occur over half way between the QRS complexes the QTc may be lengthened
- A long QTc interval (known as “long QT”) is especially important to identify in patients with a history of collapse or transient loss of consciousness.
Causes of long QT:
| Drugs | Metabolic | Familial | Other |
|
|
|
|
10. T-wave
The t-wave can be flattened or inverted for a number of reasons:
- Normal variant
- Commonly inverted in aVR and V1 and often in V2 and V3 in people of afro-Caribbean descent.
- Ischaemia
- Ventricular hypertrophy (strain pattern) usually in lateral leads
- LBBB (t-wave inversion in the anterolateral leads)
- Digoxin
- Hypokalaemia (can cause flattened t-waves)
N.B. Hyperkalaemia causes peaked T waves. The classic changes in hyperkalaemia are:
- Small p-wave
- Tall, tented (peaked) t-wave
- Wide QRS
- Widening of the QRS indicates severe cardiac toxicity
Summary
Following steps 1-10 above give the ideal system for interpreting an ECG. If you work through these steps you will be unlikely to miss anything significant.
Click here for the next section: how to identify bundle branch blocks
…and click here for medical student OSCE and PACES exam questions about ECGs