Starting non-invasive ventilation (CPAP and BiPAP)
How and when to start BiPAP and CPAP
Non-invasive ventilation (NIV) refers to CPAP and BiPAP. This page explains the practicalities of starting a patient on NIV. See the intensive care pages for details and specific indications for CPAP and BiPAP (and high flow nasal oxygen – ‘HFNO’ or ‘optiflow’)
CPAP and BiPAP basics
- CPAP (continuous positive airways pressure)
- CPAP is delivered with a tight fitting mask attached to a ventilator. It gives a continuous pressure (analogous to PEEP: positive end expiratory pressure).
- Usual settings are 5, 7.5 or 10 cmH20
- CPAP is commonly used in acute pulmonary oedema after medical management has failed
- The aim of CPAP is to splint airways, reduce alveolar collapse, enable alveolar recruitment and to increase the functional residual capacity
- BiPAP (bilevel positive airways pressure)
- BiPAP is also delivered by means of a tight fitting face mask but the ventilator delivers two different airway pressures. These are an inspiratory pressure and an expiratory pressure.
- The expiratory pressure (EPAP) is analogous to PEEP on CPAP and is usually set between 4-6 cmH2
- The inspiratory pressure (IPAP) is a higher pressure which aims to augment the patient’s inspiratory effort
- Common settings for IPAP are 12 cmH20 which can then be escalated depending on the patient response. It can go up to 20 cmH20 if needed.
- BiPAP is used to treat type 2 respiratory failure and is commonly used in exacerbations of COPD but only after full medical management in appropriate patients.
What to consider before starting NIV
- Consent
- Should be sought whenever a patient has capacity and the ability to communicate
- Future plans and ceilings of care should also be discussed with the patient and relatives where possible
- Contraindications
- There are various contraindications to NIV (see below). However, NIV may be used in the presence of the contraindications if life is threatened. Rationale should be clearly documented.
- Make a plan in case of failure
- Is the patient appropriate for ICU? What is the ceiling of care? How long will you persist with NIV if it doesn’t seem to be working?
- BTS suggest five categories of plans when starting NIV:
- If NIV fails in under 4 hours, escalate to intubation
- If NIV fails between 4-48hours, escalate to intubation
- If NIV fails NIV consider palliation if it is not appropriate to proceed to invasive ventilation
- Continue NIV if there is a response to therapy and seek specialist respiratory input with regards to duration of therapy and weaning.
- Inappropriate to commence NIV and palliate from the outset
- In addition DNAR status should be considered prior to commencing NIV. This is helpful but note that having a DNAR certainly does NOT preclude the use of NIV (or invasive ventilation).
- Monitoring
- Both CPAP and BiPAP can reduce cardiac output and cause haemodynamic instability so it is important to monitor pulse and blood pressure closely.
- Fluids and nutrition
- Whilst wearing an NIV mask the patient will have less oral intake and insensible losses will be higher.
- Monitor fluid balance and give iv fluids as necessary
- If NIV is to be worn for more than 24-48 hours then NG feeding should also be considered.
- Use the narrowest bore NGT possible to reduce mask leakage
- Whilst wearing an NIV mask the patient will have less oral intake and insensible losses will be higher.
Setting up NIV
- Explain
- NIV is unpleasant and lack of tolerance is a major reason for failure . Tell the patient about this and explain very clearly what NIV involves.
- Tell them you will start very slowly and move in steps. Acknowledge it is unpleasant but emphasise its importance.
- Prepare
- Get the correctly fitting mask to reduce any pain
- Have a nurse there who is experienced with NIV – this is absolutely invaluable.
- The pressure from NIV often leads to bloating and nausea. Give an antiemetic and consider an NGT prophylactically to reduce gastric pressure
- Put on the mask
- Start by setting up the pressure settings with the mask no on the patient.
- Position the mask near the patient’s face so they can feel the air blowing into their face without the mask touching them
- Then hold part of the mask on their face – give them time to adjust
- When ready, hold the mask to their face letting them get use to the pressure
- When they have got used to this then put on and tighten the straps to ensure a proper fit.
- You should stay with them throughout this time
- Starting NIV settings
- CPAP
- Usual settings are 5, 7.5 or 10 cmH20
- BiPAP
- The aim is to commence BiPAP at settings of 12 cmH2O/4cmH2O (IPAP of 12, EPAP of 4) and escalate the IPAP:
- Start EPAP at 4 or 5 cmH2O
- Start IPAP at 10 cmH2O titrated rapidly in 2-5 cm increments at a rate of approximately 5cmH2O each 10 minutes with a usual pressure target of 20cms H2O or until a therapeutic response is achieved or patient tolerability has been reached.
- Setting changes should be guided by serial ABGs and the respiratory or ICU teams should be involved to help guide this.
- The aim is to commence BiPAP at settings of 12 cmH2O/4cmH2O (IPAP of 12, EPAP of 4) and escalate the IPAP:
- CPAP
Monitoring of NIV
- Try to stay with the patient for at least five minutes to ensure they are comfortable. Use this time to start optimising settings
- Arterial blood gases should be taken as a minimum at 1, 4 and 12 hours after the initiation of NIV
- A decision to proceed to invasive mechanical ventilation should normally be taken within 4 hours of initiation of NIV
- Intubation where appropriate is the management of choice in late (>48hrs) NIV failures
- With both CPAP and BiPAP the inspired oxygen (FiO2) can be titrated to achieve a target PaO2 or saturations.
- Close monitoring and serial blood gases are imperative for any patient being treated with non-invasive ventilation so any improvements or deteriorations in the clinical state can quickly be identified.
How to wean NIV
- Initially weaning should be during the day with extended periods off the ventilator for meals, physiotherapy, nebulised therapy etc.
- After successfully weaning during the day, most patients will require an additional night on NIV.
- Usual practice involves a 4-day weaning period
- Day 2: Continue NIV for 16 hours (including 6-8 hours overnight)
- Day 3: Continue NIV for 12 hours (including 6-8 hours overnight).
- Day 4: NIV may be discontinued unless continuation is clinically indicated
- e.g. Two hours in the morning, two hours in the afternoon and six hours overnight
- Some patients make a rapid recovery and shorter weaning periods of 2-3 days are often reasonable
Contraindications to NIV
- Facial burns/facial trauma
- Recent upper GI surgery
- Vomiting
- Fixed airway obstruction
- Undrained pneumothorax
- Patient is unable to protect their own airway
- e.g. moribund with low GCS or copious secretions
- Life threatening hypoxaemia
- Multiple comorbidities
- Confusion and agitation (unless caused by hypoxia or hypercapnoea which would be reversed by NIV)
- Patient refusal
- Bowel obstruction
- Haemodynamic instability requiring inotropes (unless on ICU)
- NIV is not the treatment of choice for patients with consolidation on CXR but is sometimes used if escalation to intubation and ventilation is deemed inappropriate
Click here to download free British Thoracic Society (BTS) guidelines on starting non-invasive ventilation : Non-invasive ventilation
Perfect revision for medical students, finals, OSCEs and MRCP PACES
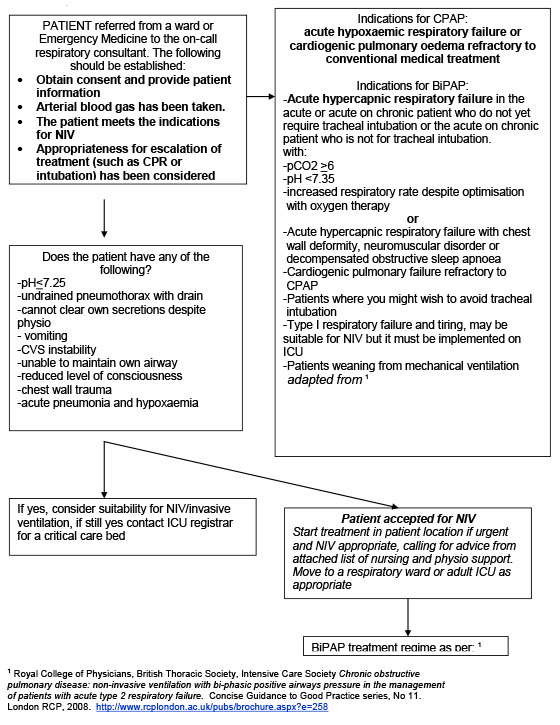
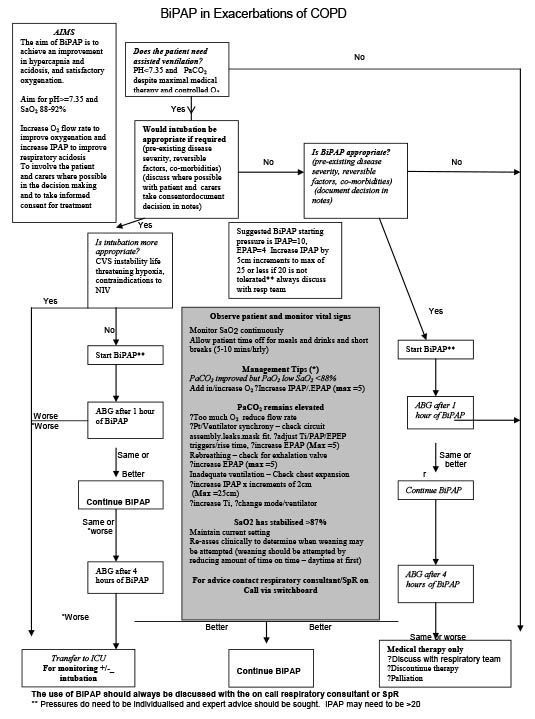
BTS guidelines on indications for NIV
BTS guidelines on starting BiPAP for COPD