Intercostal drain (chest drain / pleural drain) insertion
An intercostal drain (also known as a chest drain or pleural drain) is a flexible plastic tube that is inserted through the chest wall into the pleural space. It is used to drain pneumothoraces or effusions from the intrathoracic space. All intercostal drains inserted for pleural effusions should be real time ultrasound guided
Indications for intercostal drain insertion (chest drain/pleural drain)
- Unresolved primary pneumothorax greater than 2 cm after 2 attempts at aspiration
- Secondary pneumothorax greater than 2 cm
- Unilateral pleural effusion causing breathlessnesss – insert drain to relieve symptoms and aid diagnosis
- Empyema
- Bilateral pleural effusions if decompensated despite optimal medical management
- Tension pneumothorax after needle decompression
- Palliation of breathlessness in malignant pleural effusions
- To facilitate pleurodesis
Equipment required for an intercostal drain (chest drain/pleural drain)
- Ultrasound and operator (for effusions)
- Sterile ultrasound sheath
- Sterile field
- Sterile dressing pack and gloves
- 2% Chlorhexadine swabs
- Analgesia
- 4mls of 1% or 2% Lidocaine
- Orange (25G) needle (x1)
- Green (19G) needle (x1)
- 5ml Syringe (x1)
- Seldinger chest drain kit
- Chest drain tubing and bottle
- Sterile water/saline
- Suture kit
- Straight needle is ideal
- Sterile dressing
Contraindications to intercostal drain (chest drain/pleural drain)
- Coagulopathy
- Haemothorax (can insert a large bore Seldinger but a trauma drain may be more appropriate)
- Local infection
Pre-procedure
How to consent a patient for an intercostal drain (chest drain/pleural drain)
- Written consent should be gained for:
- Pain, failure of procedure, bleeding, infection, damage to surrounding structures and pneumothorax if the procedure is for an effusion.
Pre-procedure set-up
- Set up sterile trolley
- Prepare drain
- Pour sterile water/saline into chest drain bottle up to the prime line
- Attach chest drain tubing ensuring the end stays within the package and sterile
- Review imaging and examine patient to confirm side of insertion
- It is advised to have a nurse and a helper to assist during the procedure
- Position the patient with leaning forward with arms out stretched or sat at 90 degrees with arm lifted and hand resting behind their head. In elderly or frail patients the nurse may be required to help support this position.
- If drain is for a pleural effusion then ultrasound area to identify insertion site
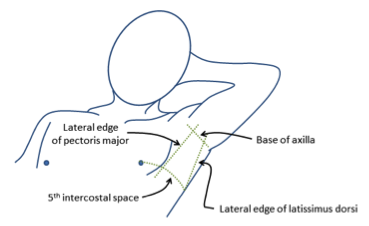
Safe triangle for chest drain insertion
Procedure for intercostal drain insertion (chest drain/pleural drain)
- Wash hands and don sterile gown and gloves
- Clean insertion site: either the site identified by ultrasound or – for pneumothorax – insert drain in the “safe triangle”
- Lower border of axilla to the 5th intercostal space; the lateral edge of pectorails major and the lateral edge of latissimus dorsi
- Apply sterile field
- Insert lignocaine cutaneously, subcutaneously and then into the pleural space.
- Fluid or air should be able to be aspirated with the green needle
- Take the Seldinger needle and attach this to the 10ml syringe provided
- Insert needle in the same plane as the lignocaine, aspirating as you advance. Insert needle to the same distance as air was aspirated with the green needle. Once air is aspirated inset 0.5cm further and confirm ongoing air aspiration
- Remove the 10ml syringe ensuing you place your thumb over the open needle
- Take the Seldinger wire and insert through the needle. Ensure you hold the wire and needle at all times
- Remove Seldinger needle over the wire
- Take scalpel and make a 0.5cm incision in the skin
- Scalpel sharp edge should always be facing away from the wire
- Take the Seldinger dilator and pass it over the wire, gently but firmly insert the dilator over the wire through the skin and intercostal muscles
- Warn the patient they will feel some pushing
- Do not be too forceful as you will kink the wire
- If the dilator is not advancing it may indicate you are pushing in the wrong plane or against bone
- Once dilated remove the dilator and pass the chest drain over the wire
- Ensure that you have a hold of the wire out the end of the drain before advancing
- Insert the drain over the wire and remove the wire
- Attach three way tap to the drain and ensure it is closed
- Then confirm air or fluid aspiration with a syringe via the 3-way tap
- Close 3-way tap once position confirmed and suture drain in place
- This needs to be firm but not pinch the skin or occlude the drain
- Dress the drain so the insertion sight is visible
- Attach drain to chest drain tubing
Post-procedure
- Place drain on free drainage but monitor closely
- If the patient has a chronically collapsed lung and you drain more than 1-1.5l in the first 24 hours there is risk of re-expansion pulmonary oedema
- Analgesia
- Post procedure CXR
- Document procedure clearly and document length of drain inserted
- Advise patient to always hold drain bottle below level of insertion
- Respiratory review and advise on onward management
In the event of failure
- Stop procedure
- Seek senior help
- Re-review imaging and patient with a senior colleague to ensure presence of fluid
- Consider further imaging or chest drain insertion in radiology
Top Tips for intercostal drain insertion (chest drain/pleural drain)
- Consent the patient for pain, failure of procedure, bleeding, infection, damage to surrounding structures and pneumothorax if the procedure is for an effusion.
- When making the incision on the skin the blade should always cut away from the wire to ensure you do not cut through it.
- NEVER LET GO OF THE SELDINGER WIRE!
Click here to download free teaching notes on intercostal drain (pleural drain/chest drain) insertion: Procedures – Intercostal drain
Perfect revision for medical students, finals, OSCEs and MRCP PACES



